In March 2021, following nearly 12 months of literature review and field research, KPMG in collaboration with Johnson & Johnson jointly release a bespoke whitepaper for Asia-Pacific leaders on the topic of Major Depression. While much progress has been made in terms of placing a level of focus on mental health and even depression in the Asia-Pacific, more will need to be done in order to truly address the rising demand for support and the “spectrum” of sub-conditions that exist within the Major Depression category; sub-conditions which cause disproportionate levels of burden and therefore must be tackled in a more targeted manner. Arguably, such a topic is even more important following the very challenging pandemic period.
We provide key excerpts of the report on this webpage, with the full document and set of analyses available for download here too. We hope the report fosters proactive public-private dialogue about Major Depression in the Asia-Pacific, and we remain available for any questions or queries on the same. Let us re-imagine a future freed from Major Depression.
About the report and its call to action
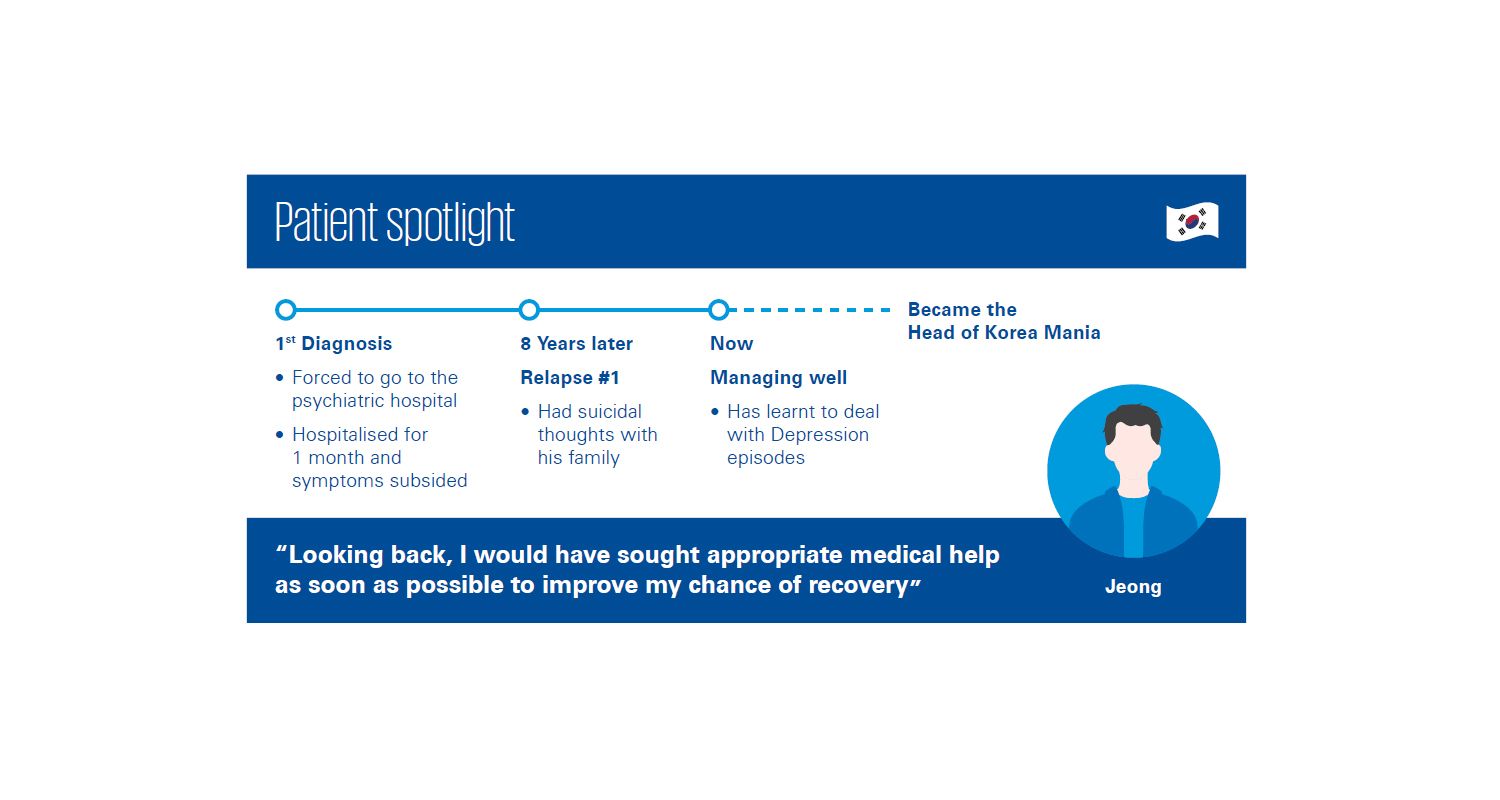
The impetus for the research stems from the rising prevalence and cost of Major Depressive Disorder (MDD) in the Asia-Pacific. Despite heightened awareness of the mental health topic, broadly-speaking, and an increase in depression-related policies, our populations continue to suffer due in large part because MDD is viewed as a homogenous disorder. In fact, MDD is a collection of symptoms, which vary at an individual level. Recognition of this reality, and applying the appropriate response, would be a great start.

Upon reviewing global best practices in addressing the spectrum of MDD, we heard from policymakers, healthcare practitioners, patients, and other stakeholders about how things are playing out in practice on the ground in the Asia-Pacific. Policy recommendations were then coalesced, so as to intervene now and to harness the evolution of our societies in the region, rather than to be burdened by it. Currently, MDD is the largest disability category among mental illnesses, and second largest overall. More targeted resource allocation will be key in achieving MDD spectrum pathway improvements.


The challenge in front of us
Around the world, 350 million people are living with depression and we lose a life to suicide every 40 seconds. Current interventions such as Cognitive Based Therapy (CBT) and Electro Convulsive Therapy (ECT) may be ineffective for certain needs along the MDD spectrum and, as a result, the rate of antidepressant medication prescription in the Asia-Pacific is increasing two-fold. 30% of people do not respond to any form of treatment, and for someone with MDD, their lives tend to be 20 years shorter than the average.
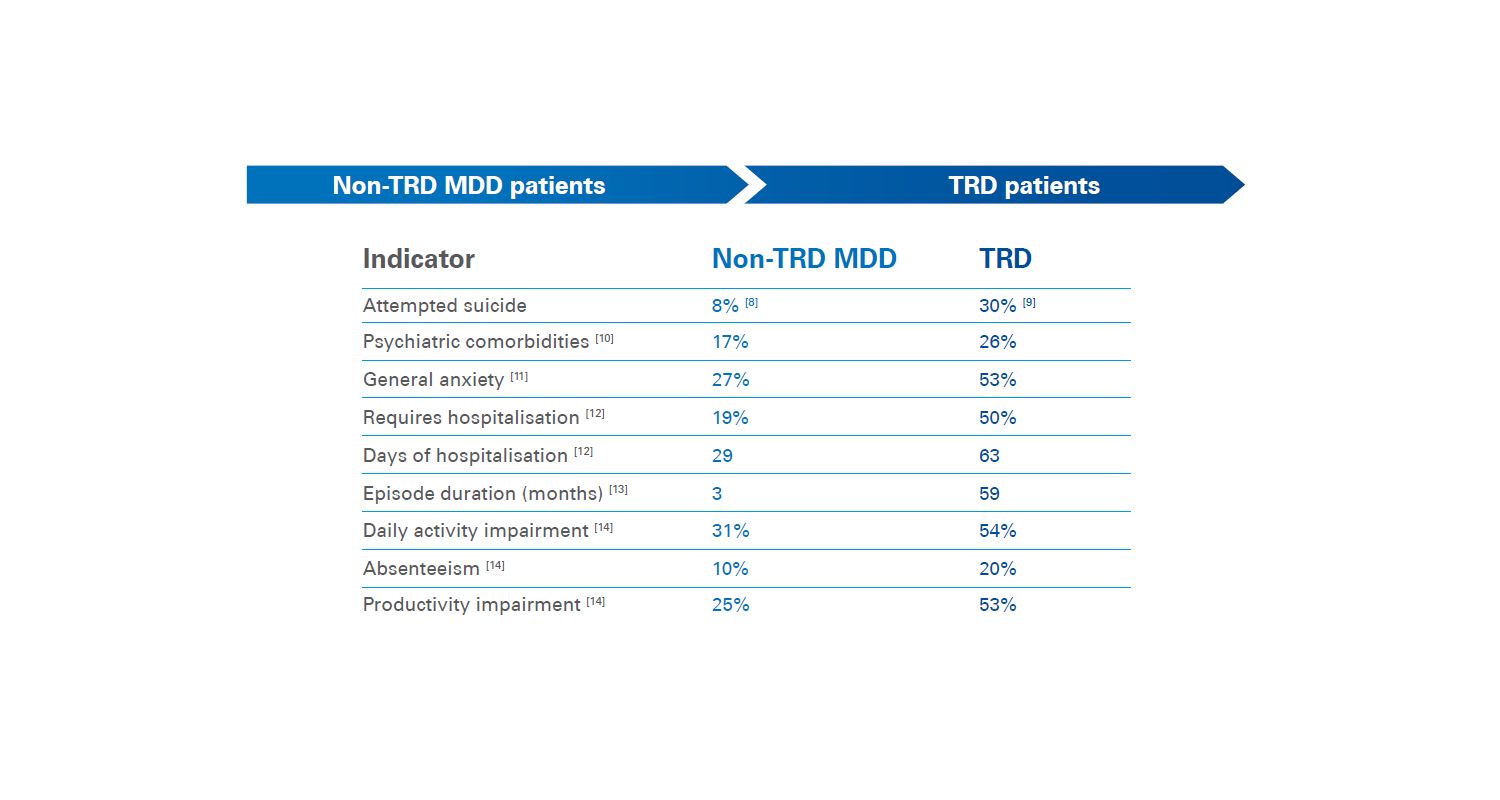
An example of a sub-condition along the MDD spectrum is Treatment-Resistant Depression, defined as MDD episodes that do not respond to at least two rounds of treatment attempts. While the measured clinical burden of TRD is about 2x that of MDD, the economic burden is 5x. Hence, a much more targeted approach to the identification and management of TRD scenarios is a critical strategy to be deployed by Asia-Pacific leaders.
The report then goes into further detail across leading indicators such as budget allocation, coverage schemes, policy attempts, and per capita resources as a type of market-specific league table in order to make comparisons across the Asia-Pacific region. The second half of the report provides market-specific snapshots outlining the respective progress made thus far and the recommended paths forward, taking into consideration local cultural context.
Clearly, in a region with health systems that are already tight on resource allocation, we must be more targeted in our efforts. MDD remains one of the leading causes of out-of-pocket healthcare expenditures, and up to 90% of people living with MDD do not seek help at all. Those with MDD are 40% less productive when not supported appropriately, meaning the economic and social impacts are adding up to the trillions of dollars in the Asia-Pacific. We must act now to make a difference.
A window of opportunity – policy recommendations to take forward
The good news for leaders in the Asia-Pacific is that we have something to teach, and something to learn from the existing good practices occurring in the region and globally. It’s a matter of doubling down and being more targeted in the effort. The report summarises the solution concepts at macro and micro levels, leveraging stakeholder contributions to help with the shaping.
The policy recommendations are primarily along the following three themes:
- Enforcing nationwide standards for MDD educational campaigns so as to improve understanding – driving more conversations through youths and influencers, requiring employers (public and private) to offer the requisite levels of support, and utilising platforms for scale such as by establishing “Depression Day”.
- Providing sustainable coverage to shift toward proper MDD diagnosis and treatment – ensuring national planning cycles account for the MDD spectrum, and formalising the recognition of caregivers and families who are supporting people living with MDD.
- Deploying new models of care that are a more effective and efficient use of resources – empowering the use of digital tools in the MDD care systems, reorganising treatment pathways to reflect a patient-centric mindset, and staying at the forefront of novel interventions.
The report concludes by proposing two possible futures – one staying the existing course and failing to achieve our population socioeconomic development ambitions due to the lingering burden of MDD; versus another incorporating the policy recommendations and creative solution concepts, upon which populations become freed from MDD. Certainly, we must aim for the latter, which necessitates a greater understanding and bias for action toward addressing MDD as a spectrum.