What is changing in healthcare reimbursement?
With the introduction of mandatory health insurance underway in the public sector in the Kingdom and the wish to standardize across the public and private sector, Saudi healthcare providers will need to develop new capabilities to be able to generate revenue under the new reimbursement system.
As part of Vision 2030 and the National Transformation Program, Saudi Arabia’s healthcare sector is undergoing a major transformation that will significantly change the reimbursement system of health services. The Ministry of Health (MoH) is aiming to change its role from being an all-in-one payer, provider and regulator of health services to becoming a regulator, governing corporatized payers and providers. A key aspect of this transformation is the separation of the payer and the provider functions in the public healthcare sector. To facilitate future reimbursement to Public Healthcare providers, the Ministry of Health has set up the Program for Health Assurance and Purchasing (PHAP). In addition, the Council of Cooperative Health Insurance (CCHI) has also firmed up regulations for private insurers.
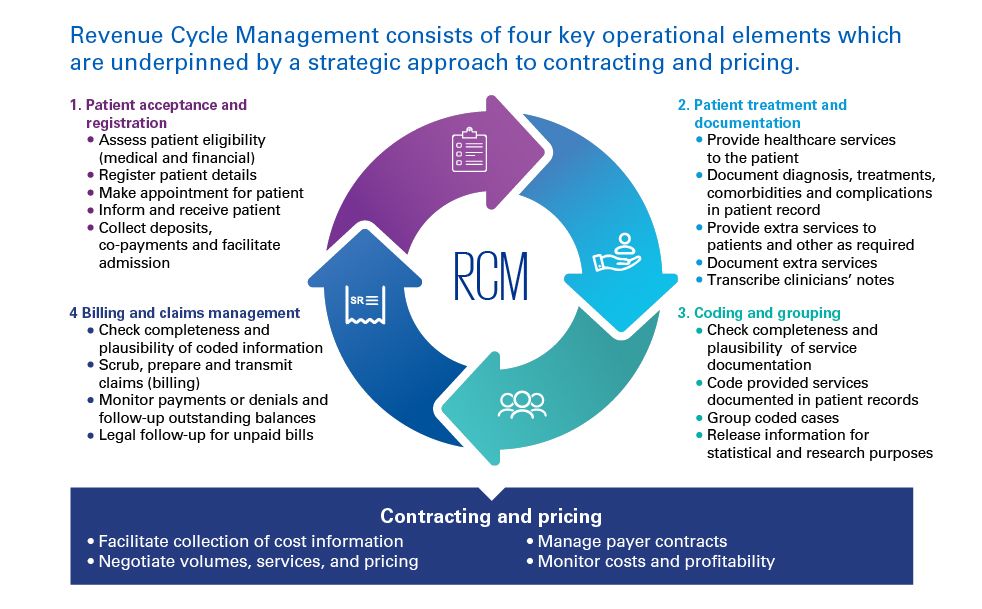
Under the new reimbursement mechanism, healthcare providers will need to be able to, among other things:
- Raise invoices to payers (e.g. insurers, self- paying patients, corporates) for each episode of treatment
- Assure the integrity of their income Generate data to negotiate with payers
- Use data to improve their cost efficiency and service quality to compete with other providers.
This is a significant change in how income has been received by most providers to date in the Kingdom, and will require providers to both undergo a significant culture shift and develop new capabilities, including, but not limited to:
Determining which patients are medically and financially eligible prior to registering patients under the new system
- Repeating the check prior to each appointment/ treatment episode
- Documenting the services provided to their patients accurately and correctly
- Coding and grouping services provided in new ways
- Raising bills according to the contractual terms to both new and existing payers, as well as managing and following up on claims
- Understanding the true costs of healthcare services to support more informed pricing negotiations with payers
The processes to perform these tasks, together, are referred to as Revenue Cycle Management (RCM) which is the subject of this report.